by BC Advantage
Nov 29th, 2016
If E/M stands for "evaluation and management," E/M coding is the process by which provider-patient encounters are translated into five digit CPT codes to facilitate billing. CPT stands for "Current Procedural Terminology." These are the numeric codes which are submitted to insurers for payment. Most billable procedures have their own CPT codes. Some procedures are new or unusual so they use unspecified codes.
The CPT codes which describe provider-patient encounters are often referred to as "E/M codes." There are different E/M codes for different types of encounters such as office visits or hospital visit. There are different E/M codes for different types of encounters, such as office visits or hospital visits. Within each type of encounter, there are different levels of care. For example, the 99214 code may be used to charge for an office visit with an established patient. There are five levels of care for this type of encounter: 99211 - 99215.
The 99214 code is often called a "level 4" office visit because the code ends in a "4" and also because it is the fourth "level of care" for an established patient visit.
Each patient encounter should be carefully documented in the patient chart.
The documentation for E/M services is based on three "key" components, History, Physical Exam and Medical Decision Making. The key components are used to satisfy the documentation requirements for E/M coding.
The E/M key components can be thought of as the building blocks of documentation for all patient encounters. Some types of encounters require complete documentation of all three key components, while others require only two out of three.
HISTORY - is a narrative in the patient's own words which provides information about the clinical problems or symptoms being addressed during the encounter. As the history increases in intensity, so does the level of care. The history is composed of four building blocks.
1. Chief Complaint (CC) - A concise statement in the patient's own words that describes the symptom, problem, condition, diagnosis, or reason for the patient encounter. In an audit payment for services can be denied simply because the chart note did not include a chief complaint.
2. History of Present Illness (HPI) – A chronological description of the development of the patient's present illness from the first sign and/or symptom or from the previous encounter to the present.
HPI elements are:
- Location
- Quality
- Severity
- Duration
- Timing
- Context
- Modifying Factors
- Associated Signs and Symptoms
There are two types of HPI:
a. Brief HPI – includes documentation of one to three HPI elements.
b. Extended HPI - According to the 1997 guidelines, at least four elements of the present HPI or the status of a least three chronic or inactive conditions.
3. Review of Systems (ROS) - An inventory of specific body systems discussed by the physician or medical assistant in the process of taking the history from the patient. The ROS is designed to bring out clinical symptoms which the patient may have overlooked or forgotten. In theory, the ROS may illuminate the diagnosis by bringing out information which the patient may not perceive as being important enough to mention to the physician.
b. Extended HPI - According to the 1997 guidelines, at least four elements of the present HPI or the status of a least three chronic or inactive conditions.
3. Review of Systems (ROS) - An inventory of specific body systems discussed by the physician or medical assistant in the process of taking the history from the patient. The ROS is designed to bring out clinical symptoms which the patient may have overlooked or forgotten. In theory, the ROS may illuminate the diagnosis by bringing out information which the patient may not perceive as being important enough to mention to the physician.
There are fourteen individual systems recognized by the E/M guidelines:
- Constitutional (e.g., fever, weight loss)
- Eyes
- Ears, Nose, Mouth, Throat
- Cardiovascular
- Respiratory
- Gastrointestinal
- Genitourinary
- Musculoskeletal
- Integumentary (skin and/or breast)
- Neurological
- Psychiatric
- Endocrine
- Hematologic/Lymphatic
- Allergic/Immunologic
4. Past, Family and Social History (PFSH) - Is a review of three history areas:
- Past history
- Family history
- Social history
PHYSICAL EXAM - Unlike the key components of history and medical decision-making, the rules defining the various levels of physical exam are quite different for the 1995 vs. the 1997 E/M guidelines. The 1995 E/M guidelines allow the physician to complete the physical exam by documenting organ systems or body areas. This approach is quite subjective and gives physicians a lot of leeway and "wiggle room." On the other hand, the 1997 E/M guidelines are quite rigid and force physicians to document the exam using specific bullets. The 1997 physical exam rules are much more "black and white" so it is easier to defend your position in an audit.
The E/M guidelines recognize levels of exam:
1. Problem focused - A limited exam of the affected body area or organ system.
2. Expanded problem focused - A limited exam of the affected body area or organ system and other symptomatic or related organ system(s).
3. Detailed - An extended exam of the affected body area(s) and other symptomatic or related organ system(s).
4. Comprehensive - A general multisystem exam or a complete exam of a single organ system.
2. Expanded problem focused - A limited exam of the affected body area or organ system and other symptomatic or related organ system(s).
3. Detailed - An extended exam of the affected body area(s) and other symptomatic or related organ system(s).
4. Comprehensive - A general multisystem exam or a complete exam of a single organ system.
MEDICAL DECISION MAKING (MDM) - This is arguably the most important of the three key components because the MDM refers to the complexity of establishing a diagnosis and/or selecting a management option which is determined by the following factors:
- The nature and number of clinical problems
- The amount and complexity of the data reviewed by the physician
- The risk of morbidity and mortality to the patient.
There are four levels of MDM of incrementally increasing complexity:
- Straightforward
- Low Complexity
- Moderate Complexity
- High Complexity
The documentation requirements for each individual E/M code are dictated by a set of rules called the E/M guidelines. The E/M guidelines were developed by the Center for Medicare and Medicaid Services (CMS) in conjunction with the American Medical Association.
Two versions have been released; the first in 1995 and the last in 1997.
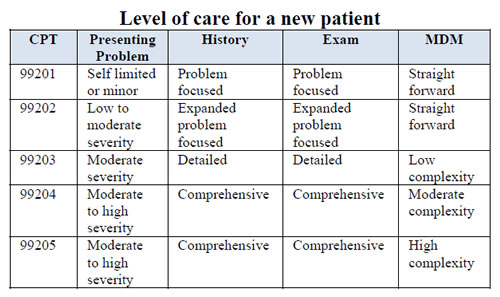
In the example above, codes 99201 - 99205 are known as new patient codes. New patients have not been seen by the practice for the past 3 years. And the rule for a new patient is they must meet 3 of 3 components from the grid above.
For example: Patient was seen for a detailed history, detailed exam, and straightforward medical decision making. Reading to the left a detailed history would give you a 99203; a detailed exam would be a 99203; but a straightforward medical decision making would only give you a 99202. Since all three must be met to choose the code, the highest possible code we could choose would be a 99202 due to the medical decision making.
The E/M guidelines define the requirements for individual E/M codes based on the extent of the documentation of the three key components. In general, higher paying E/M codes (like consultations or initial office visits) require more extensive documentation than lower paying codes (such as office visits with established patients or hospital progress notes).
See more at BC Advantage
 Quick, Current, Complete - www.findacode.com
Quick, Current, Complete - www.findacode.com