by NAMAS
Aug 2nd, 2019
Who knew that when Jack & Jill when up the hill to fetch a pail of water, they would have to ensure that in order to keep the level of water the same on the way back down, they would need to both support the pail.
Many of you in this industry are also tasked with "supporting the level in the pail," or for that matter, multi-pails. We all know the challenges of being tasked daily with Clinical Documentation Improvement (CDI) audits and that a primary focus of these audits is ensuring that the coding and documentation supports the level of service.
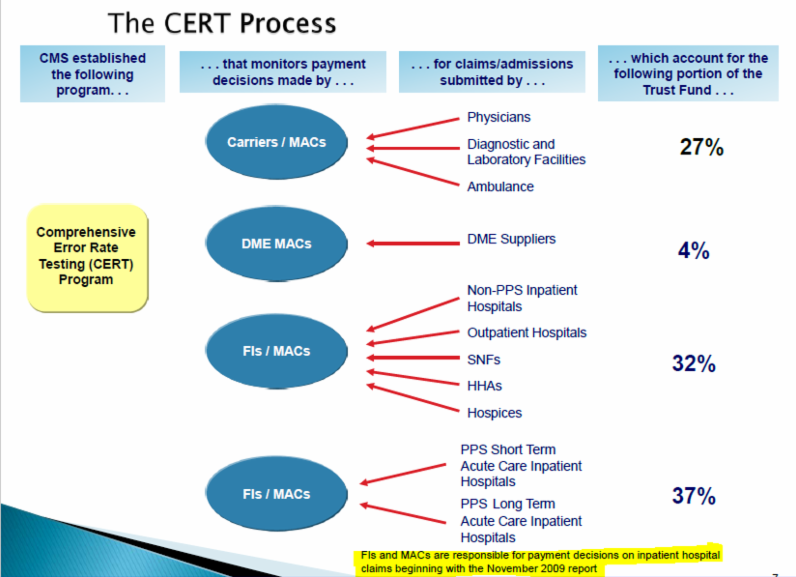
Every November, the Department of Health and Human Services (HHS) makes public its annual Improper Payment Rates for the prior year. Contained within this is the Comprehensive Error Rate Testing (CERT) program. The list also contains the Annual CMS Fee-for-Service (FFS) Improper Payments Report. The CERT reports are designed to monitor claim payment accuracy of the CMS FFS program, in order to protect the integrity of the Medicare Trust Fund. The CERT report identifies types of errors and assesses error rates at both national and regional levels in all types of healthcare settings in the U.S. The CERT report drills down into the errors and can hone in on specific provider types or services and also allows CMS to evaluate the performance of Medicare Administrative Contractors (MACs), such as CGS, Noridian, FCSO, and others around the country.
Where does the industry stand with respect to overall levels of care in the vast majority of services provided? How can we tell if our trips up and down the CDI hill are paying off? Well, CERT is one of several great tools that CMS publishes on their website (link below) that everyone can access. The CERT reports show us what CMS has found trending in overpayments to the healthcare industry, year to year and in what areas they are commonly occurring. This is a great forecast of future audit areas and can help you focus CDI efforts within your practice/entity.
About NAMAS
NAMAS is setting the standards in medical auditing & education
The NAMAS team and faculty work hard to bring you membership resources, products, tools, and training that is not only timely and specific to medical auditing and compliance, but also that is specific to the needs of medical practices today. NAMAS staff are industry recognized experts who provide audits and consulting services to active clients which gives NAMAS the cutting edge to provide relevant training.
The Slippery Slope For CDI Specialists. (2019, August 2). Find-A-Code Articles. Retrieved from https://www.findacode.com/articles/the-slippery-slope-for-cdi-specialists-35032.html
© 2019 InnoviHealth Systems Inc

 Quick, Current, Complete - www.findacode.com
Quick, Current, Complete - www.findacode.com